|
The CHAIM Centre is looking to fill 6 graduate mentor positions for the 2021 One Health Student Challenge!
Graduate Mentors are expected to guide interdisciplinary teams of undergraduate students throughout the competition as they develop an intervention to address a One Health issue facing our world today. This year’s Challenge will be fully virtual to comply with COVID-19 restrictions. Mentors must be present at the opening (January 29th, 2021), consultation session (March 5th, 2022), and closing (March 19th, 2021) online sessions. They are also expected to attend their team’s group meetings, act as a sounding board for ideas, mediate conflicts when necessary, offer resources to students, and communicate any questions students have to the organizing committee of the competition. Each position will be compensated $800 at the end of the competition in the form of a stipend. To apply, applicants must be a registered graduate student at Carleton University and send a resume and cover letter to chaimcentre@carleton.ca by December 10th, 2020. Click here for more information on the mentor position!
0 Comments
Claire Tizzard, Carleton University Graduate  London, Ontario. October, 2020 London, Ontario. October, 2020 The COVID-19 pandemic has changed the way we think about a lot of things including the way we travel, how we shop, and even where we live. Early on, as the pandemic containment measures were announced, it seemed that those who could were trading in their urban lives for the peace and tranquility of their rural cottages. Inspired, perhaps, by the wish to escape the higher transmission rates in urban centers but also the increasingly strict restrictions on public space. Those who longed for nature were encouraged to seek rural areas and homes with private backyard space in place of their urban apartments. Given that this is not an accessible option for most people, the role of urban development in the promotion of resilience and well-being has been brought into sharp focus. The thought of urban development might elicit images in our minds of new apartment buildings with large windows and rooftop patios, and while this is not the extent of urban development, it does make up an important part. The architectural features of our living space contribute to our mental health and wellbeing, particularly when we face restrictions on our ability to leave these spaces. The loss of daily routine, social gatherings, and the amalgamation of home and workspace have had a significant impact on mental health and wellbeing, all of which are compounded for those in densely packed urban areas.  A study conducted in Northern Italy, a region that experienced severe lockdown restrictions due to COVID-19, looked at the impact of features of built living spaces on university students found that living in small apartments, lacking a functional balcony, and having a poor view were each associated with moderate to severe depression symptoms (1). These living features are not uncommon as we experience a global trend of movement to urban centers where space is limited. To combat these negative psychological effects, people took to parks and local greenspace. A study that analyzed data from the Google Community Mobility Report found an increase in park visitation from February to May 2020, by over 100%, compared to the same time period the previous year, in Canada, Denmark, and the United Kingdom. Similar increases were found in Spain and Italy once the most strictest lockdown restrictions were lifted (2).  Time outdoors appears to be an important coping strategy. Nature provides an escape from confined living quarters and a time of relaxation to release the stress and anxiety felt most acutely by those in urban centers. Urban greenspaces are not only places to enjoy nature and physical activity but are also places to enjoy social connection. Community gardens and parks help foster social ties that can be maintained safely during social distancing measures to further reduce feelings of isolation and loneliness and foster resilience in a community. A survey of Tokyo residents explored the relationship between mental health scores, outdoor experience, and lifestyle factors to further understand their interaction amidst the increased psychological stress of the coronavirus pandemic. They found that greenspace use and view were both individually associated with higher life satisfaction, happiness, and self-esteem scores. Greenspace use and view were also both independently associated with lower loneliness, depression and anxiety scores (3). This supports the importance of greenspace in maintaining our mental health and wellbeing through periods of significant stress. However, greenspace is not equally accessible. Data from the Google Community Report found that park visitation and access were correlated with economic, cultural, and social dimensions. Higher socio-economic status communities experienced greater park access and visitation rates, while poverty and unemployment were correlated with reduced park access and visitation (2). Wealthier areas tend to have a greater diversity of species, higher tree cover, and are therefore, less susceptible to environmental changes (4). This inequality in greenspace access could compound the negative effects felt by disadvantaged populations due to COVID-19. Recognizing these data is important in our understanding of the impact of urban development on our wellbeing, especially as we prepare for future pandemics where quarantine measures may again be necessary for preliminary containment. Architectural design should include consideration of living features that have been found to be correlated with positive mental health and wellbeing such as a livable balcony, increased natural lighting, and larger and more functional space, all of which are a function of access to resources and socio-economic status. In addition, urban nature protection and development should be a priority as they have been shown to protect mental wellbeing and foster resilience in communities. Focus should also be brought to increasing equity in the distribution of urban nature development to benefit lower socio-economic communities who are at an increased risk of experiencing negative impacts to wellbeing.  The COVID-19 pandemic has changed the way we think about a lot of things, including how we appreciate urban greenspaces. They are no longer simply spaces that we enjoy individually, but have become crucial to maintaining our mental health and wellbeing. Urban greenspaces are places for physical activity, stress relief, and community interaction, all of which are key to combatting feelings of loneliness and isolation during lockdown restrictions. As we prepare for future pandemics, urban development that prioritizes greenspace is fundamental to fostering resilience in those who live in urban centers. References:
This blog was originally written as part of the HLTH5402 course.
This project, Diversity and Inclusion Teaching and Research Considerations at Carleton University, aims to understand student experiences and perspectives on ethno-racial diversity at Carleton. Currently, we are looking for participants to help us understand this process.
You will be asked to complete an online survey that will take approximately 15-20 minutes, and your responses will be confidential. As compensation you will be entered in a draw to win an e-gift card of CAN $100 for Amazon for completing the survey. If you are among the first 50 participants, your chances of winning the prize are 1 in 50 in the first draw, 1 in 100 in the second, and you’d be entered in a third draw as well with a 1 in 150 chance of winning. Your participation at each time point is entirely voluntary, and you may withdraw at any time. To be eligible, you must be a current Carleton University undergraduate student or recent alumni (Class of 2021) and be fluent in English. There are no physical risks in this study, but you may experience mild discomfort when responding to questions asking for your experiences related to ethno-racial considerations. If you are interested, please go to: https://carletonu.az1.qualtrics.com/jfe/form/SV_3xiEw3ZQaY6t5mC or email Melissa Carvalho at melissacarvalho@cmail.carleton.ca or Jyllenna Landry at jyllennalandry@cmail.carleton.ca. You may also contact Dr. Kim Matheson at kim.matheson@carleton.ca. The ethics for this project have been approved by the Research Ethics Board at Carleton University (Clearance #115985). If you have any ethical considerations about this study, please contact the Carleton University Ethics Board-B by email at ethics@carleton.ca.  Hilary Ziraldo, Carleton University Student On the day I wrote this, exactly one year had passed since the World Health Organization declared COVID-19 a global pandemic. Like every other day that year, I was at my home in Toronto, only leaving to get groceries or to exercise outside. When I ran into my mom as she headed down the stairs to her basement work-from-home setup, she liked to joke that there was “heavy traffic” on her morning commute. Joking aside, COVID-19 has changed how we interact with our physical environments. We have become increasingly dependent on our homes and neighbourhoods to support our physical and mental health needs, and this has intensified health disparities between those living in adequate and inadequate conditions. The impacts of housing on health are numerous. Overcrowding can increase the spread of communicable infections, while chronic diseases, such as asthma, are associated with substandard heating, insulation and dampness (1,2). Unsafe or unaffordable housing is also a source of chronic stress and can lead to social isolation and poor mental health (2,3,4). Despite these broad consequences, 15.3% of Ontario households live in unsuitable, inadequate or unaffordable conditions, and affordable housing has been consistently de-prioritized by the provincial government (5). I find this alarming because housing is an essential human right, yet continues to be treated as non-essential by government decision-makers and the voting public. Due the high rates of poor-quality and unaffordable housing in Ontario, stay at home orders during the COVID-19 pandemic confined many Ontarians to unhealthy living conditions. Essential workers are also impacted because income is a determinant of housing quality, and the reality is that many frontline jobs are poorly compensated (6). For essential workers living in crowded or intergenerational households, continuing to work puts themselves and their families at greater risk due to both workplace exposures and their household conditions. Beyond housing, our neighbourhoods can have a large impact on health. Residents are more likely to be physically active in safe, walkable neighbourhoods and to choose healthy foods when they are easily accessible (7,8). In neighbourhoods designed to facilitate gatherings, residents perceive greater social support and a stronger sense of community belonging (8). Due to the impact of neighbourhood features on health, vast disparities in health may occur between otherwise geographically close communities. Like quality of housing, quality of neighbourhoods is largely determined by income (6) and this cannot be fixed by simply investing in the development of low-income neighbourhoods. When lower income neighbourhoods are revitalized, gentrification may occur. Gentrification refers to the transformation of the social, economic, cultural, physical and demographic features of a neighbourhood, and often leads to the displacement of long-term and socially marginalized residents (9). In a neighbourhood impacted by gentrification, property and rental values are inflated, pushing vulnerable populations to relocate.  However, there are ways to break the cycle of revitalization and displacement caused by gentrification. The City of Ottawa is incorporating public health concepts into urban growth strategies by creating ‘15-minute neighbourhoods’ (10). A 15-minute neighbourhood is one in which all (or most) daily needs can be accessed within a 15-minute walk from one’s home. The goal of a 15-minute neighbourhood is to reduce reliance on vehicles, increase social connections, and promote equity through improved access to daily needs (10). At the provincial level, Ontario has tried to combat income-based disparities in access to healthy built environments through inclusionary zoning regulations (11). Inclusionary zoning is a strategy to increase affordable housing in desirable neighbourhoods. Under an inclusionary zoning system, every new housing development must be mixed income, meaning that a range of income levels can afford to live in high-quality housing within updated neighbourhoods. Inclusionary zoning has shown some success in the United States, but there is concern that provincial actions will be ineffective at the municipal level. Under the current system, the power to enforce inclusionary zoning lies with municipal governments, that will need to implement bylaws and regulations surrounding the construction of affordable housing units (12). By leaving decisions on inclusionary zoning to municipalities, substantial changes are not guaranteed. 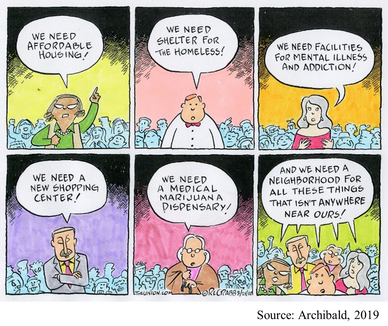 When we understand the magnitude of Ontario’s housing crisis, it is easy to support policy action, like inclusionary zoning. But, take a moment to consider your perspective if affordable housing was proposed in your own neighbourhood? As is too often the case, such a policy might be easy to support until you are personally affected. For residents living near areas allocated for affordable housing, the “not in my backyard” (NIMBY) phenomenon is both common and predictable. The NIMBY phenomenon refers to the opposition of new developments by residents when they believe the development will negatively impact their neighbourhood or property value. Classical examples of the NIMBY phenomenon include responses to safe injection sites and homeless shelters, but affordable housing is similarly affected (13). NIMBY responses are often founded in stereotypes and stigma and serve to perpetuate social inequities. One method governments and developers can use to fight the NIMBY phenomenon is to engage and inform residents throughout the planning process. Importantly, we can individually work against NIMBY-ism by discussing the value of diverse communities with family, friends, and neighbours and being leaders for social equity within our own neighbourhoods. As I sat at my desk in Toronto with the entire province under stay at home orders, I couldn’t help but appreciate how much I relied on my home and neighbourhood over the past year. But, for many Ontarians, hiding away at home has not been a refuge from the dangers of COVID-19. Improving access to healthy homes and neighbourhoods is a complex battle involving political priorities, revitalization and gentrification, and local sentiments. As we move forwards in the COVID-19 pandemic and into its aftermath, we must do more to ensure that “home” is a healthy environment for all Ontarians. References:
This blog was originally written as part of the HLTH5402 course.
|
Archives
March 2023
Categories
All
|

 RSS Feed
RSS Feed