Viral : Ability of a virus to infect, cause disease and spread from host to host.
Microbiota: Collection of microbes: bacteria, viruses, fungi, etc., specific to gut and lungs.
Leaky Gut: Increased permeability of the gut barrier, can contribute to cytokine storm by increasing viral & bacterial invasion into circulation and promoting inflammation.
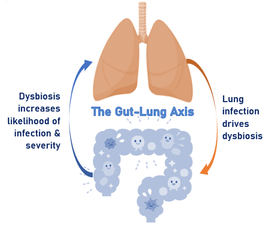
Dysbiosis: General term for a microbiome characterized by
increases in pathogens and loss of beneficial bacteria. Promotes
inflammation and leaky gut.
Cytokine Storm: Release of many proinflammatory signals (cytokines). When prolonged it causes damage to cells and organs.
Genera, Species, & Strain:
The order that the tree of life categorizes organisms into groups starting from general shared genera to specific unique strains.










 RSS Feed
RSS Feed