|
Angel Xing, CHAIM Centre Communications and Strategy Intern  Three CHAIM Centre Affiliates shared their experiences as Asian researchers for Asian Heritage Month in May, discussing social and cultural health inequities, particularly in mental health. Dr. Melissa Chee, an assistant professor in Carleton's Neuroscience department and principal investigator at The Chee Lab, said she started reflecting more on how her Southeast Asian identity affects her professional career when the 2020 Black Lives Matter movement sparked discussions about systemic racism. "It's still a discovery process for me," she said. "I know that lately I've been more aware, and I sometimes pause to ask; am I not part of that, or am I part of that because I'm Asian?" Asians are often treated as the "model minority," a stereotype that characterizes Asians as academically and economically successful compared to other minority groups. According to an article by NPR, this undermines anti-Asian hate and creates a racial divide. Dr. Chee commented on the impact of this stereotype. "Asian women are actually underrepresented in science, and I feel I need to succeed in my role so others will continue to have the same opportunity," she said. Ajani Asokumar, who identifies as Tamil and is currently pursuing her Ph.D. in Neuroscience at Carleton, agreed. "It made me really nervous because I have these expectations and pressures on me that I have to fulfill," she said, adding that sometimes she felt like she was being treated differently in academic and social settings. "You can detect it in the comments people make." In addition to the pressures, Asokumar also pointed out that Asian immigrant families don't often discuss stress and mental health, both heavily stigmatized topics. "In the Asian cultures typically, mental ill health is looked upon as almost shameful, a reflection of laziness," said Dr. Zul Merali, former scientific director of the University of Ottawa's Institute of Mental Health Research. Dr. Merali identifies with the South Asian community. "But mental illness is an illness like any other," he said. "It is not something you need to blame yourself for." Unfortunately, the pressure from Asian stereotypes combined with cultural mental health stigmas makes the Asian community more vulnerable to poor mental health. In 2016, CAMH reported that Chinese and South Asian patients had more severe mental illnesses when they were admitted to the hospital. Another issue the CAMH report identifies is that there is limited data on Chinese and South Asian patients in mental health research and general health research. Dr. Chee and Asokumar said an issue lies in the "Asian" categorization. "The Asian community is really diverse in Canada," Dr. Chee said. Besides different ethnicities and cultures, variables also include time spent in Canada and language barriers. "The experiences of someone new to Canada are very different from my experiences. I've been here my whole life." Asokumar added that mental health help is often only designed for Western people and feels alienating because the professionals don't have the same cultural understanding. "The help that's given is so general," she said. "We need better access to people who are better suited to help our needs." "When you present an opportunity, it might not be accessible to everyone equally." Dr. Merali said there are also great challenges in getting admission and treatment into the healthcare system, particularly for mental health, because the system is under-resourced. He said this affects all marginalized groups, especially because support like psychological counselling often requires private insurance. "All marginalized populations pay the price," he said. Since people from these communities cannot access mental health resources as easily, Dr. Merali said they are underrepresented in collected data for mental health studies. That said, Asokumar said she does feel like there are more people of colour in her program than there were in 2013 when she first came to Ottawa. She said there had been significant changes compared to when she was one of the few people of colour in her program. "I'm seeing more people who look like me, so it's a very positive thing that's happening," she said.
But she said she still sees mostly white men in authority positions. "I think more needs to be done. I do want to see more action," Asokumar said. Dr. Chee agreed there should be an increase in the diversity of people who sit on committees. "It's always on the back of your mind whether you were included because you're the token minority. Was I included because I am a minority and a woman? Or was I included because of my ability or expertise?" "We don't know whether our identity has hindered our ability to accelerate in our field," Dr. Chee said. "We think that we are here because we earned and deserve it, but how do we know that we didn't deserve more?" "We need more research. We need information and advocacy."
0 Comments
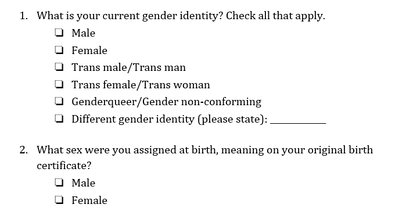
 Genderqueer Pride Flag Genderqueer Pride Flag Jaya Rastogi, Health Science, Technology, and Policy MSc Student “For me, going to the doctor is scary and dangerous,” said a genderqueer undergraduate student accessing healthcare in Ontario. “I called my family doctor to ask about [a health service that is unique for genderqueer individuals]. He said ‘I’ve never heard of that. What is that? I don’t know how to do that.’ This says to me that my doctor hasn’t educated himself enough, which seems irresponsible.” The genderqueer and trans community Genderqueer and trans individuals face unique barriers when accessing health care. In 2018, Carleton University’s independent newspaper, the Charlatan, reported on an Algonquin College student, Ashton Schofield, who faced multiple challenges accessing trans-inclusive healthcare in Ottawa. He faced numerous barriers to care including limited providers with enough knowledge to treat trans patients, long wait times for the limited providers, and an incorrect hormone medication prescription (1). Schofield’s story is not unique. As many as 1 in 200 Ontarians are trans and 11% of LGBTQ+ youth are genderqueer/gender nonconforming (2,3). Like Schofield, both genderqueer and trans individuals often face challenges accessing healthcare (4). Genderqueer is a term used to describe an individual who does not conform to one of the two binary genders⁵. Trans is an umbrella term used to describe people who move away from the gender they were assigned at birth (5,6). Some genderqueer individuals identify as trans, while others do not (7). Barriers to access and exclusion from healthcare Genderqueer and trans communities face several barriers to accessing trans-inclusive healthcare in Canada, including a lack of relevant and easily available information, self-esteem and mental health issues, challenges finding help, and ongoing experiences of transphobia (8,9). Genderqueer individuals face health-related challenges at even higher rates than binary trans people, including avoiding care due to a fear of discrimination and providers refusing to treat them (10). Genderqueer young people are becoming increasingly visible in healthcare and our communities but are paid little attention when it comes to their unique healthcare needs (9). Trans and genderqueer Canadians also experience social exclusion from healthcare (8). Many medical clinics only have male and female washrooms (11), which communicates to genderqueer individuals that their identity is not welcome in the space. Medical intake forms typically ask patients to select their sex and provide the options of male and female without asking about gender or providing any space for further elaboration (11). This says to genderqueer individuals that their identity is not acknowledged or respected in the health system. Commenting about health intake forms, the genderqueer youth quoted earlier said, “the last medical form I filled out was a form for a blood test and the options were male and female. Since I’m genderqueer I think female and male are just two really small categories.” They continued, “it’s very hard for others to respect me being androgynous. Being genderqueer is the most freeing thing because I’m not confined to these little boxes of sex or gender. Scientists and doctors are supposed to help me, but they’re the ones confining me to these little boxes. They’ll say, ‘you have to pick one or we’re going to pick for you.’ ”  Improving health intake forms Health forms are not set in stone and should be improved to better serve the genderqueer and trans community. Improving health forms is an important step in breaking down barriers to care for genderqueer and trans individuals. A recent Ontario Medical Association (OMA) report (2020) highlighted that a number of factors can lead trans youth to avoid health care (13), including the system’s focus on the gender binary and medical intake forms that ask only if a patient is male or female. A majority of trans youth criticized medical forms for being very male/female centered in a recent Manitoba-based study on trans youth’s experience in the healthcare system (12). Improving health forms would generate accurate data and provide visibility to the genderqueer and trans community. Demonstrating that genderqueer and trans people exist in local hospitals, medical clinics, and communities is important when advocating for inclusive policy, inclusive program creation and funding, and other resource allocation (12,14). The 2-step method for asking sex and gender One tool to improve visibility and accessibility in healthcare is the 2-step method for asking sex and gender, which was developed by the Gender Identity in U.S. Surveillance Group (14). This 2-step method would replace the current 1-step method that only asks a person’s sex and offers male or female as the only response options. In the 2-step method, individuals would be able to differentiate between their sex assigned at birth and their current gender identity while also having multiple options to select for current gender identity. See below for 2-step sex and gender questions (7):  Progress Pride Flag Progress Pride Flag This 2-step method was originally created for surveys but is also recommended for use in health intake forms (15). Recent Canadian research found that the 2-step method captures genderqueer and trans people’s identities better than the 1-step method, validates these identities, and was not confusing to people who are not trans (also called cis) (7). However, the 2-step method was not sufficient for some Indigenous people, and other response options may need to be added to the questions, such as two-spirit (7). There is not enough research to understand if intersex people find that the 2-step method correctly captures their identities (7). Intersex refers to individuals whose hormones or chromosomes create characteristics that are not consistently male or female (7). Additionally, some scholars argue that sex and gender markers should be eliminated wherever they are not necessary (2). While more work needs to be done to ensure questions about sex and gender accurately capture genderqueer and trans peoples’ identities, implementing the 2-step method in health intake forms is a promising step towards making healthcare more accurate and validating for trans and genderqueer individuals.
By Vinussa Rameshshanker, Carleton University Graduate Student  On April 20th, 2021, former police officer Derek Chauvin was found guilty of manslaughter as well as second- and third-degree murder of African American George Floyd last Summer.¹ What began as another instance of institutional racism within the American policing system erupted into an unprecedented, powerful global movement to recognize and transform the systemic discrimination and institutional violence that has disadvantaged people of colour throughout history. Structural racism has been front and center in recent months, referring to the pervasive inequities within the political, economic, and social systems that shape our lives.² Structural racism has repeatedly upheld ‘white privilege’ (both intentionally and unintentionally) at the expense of disadvantaging people of colour in terms of how they live, the opportunities they have access to, and ultimately their wellbeing and quality of life. Race – one of our strongest defining qualities – is a social determinant of health and wellbeing because of the systems we live in. We see racial inequities in all facets of life, whether it be access to safe and secure housing, quality education, or healthcare. We see it now as the COVID-19 pandemic rages on. One year into the pandemic, Canadian communities with the highest concentrations of visible minority populations have had roughly twice the mortality rates of communities with the lowest proportions of racial minorities.³  Without a doubt, yet another aspect of structural racism integral to our wellbeing lies within the systems through which we access food. The time for racial food justice is now. Food justice necessitates questioning the inequities, including those related to race, that structure who produces food, who has access to healthy and nutritious foods, and the kinds of food we eat to nourish us throughout our lives.⁴ We all have the right to adequate food, and the implications of having access to quality nutrition, from childhood to our later years, can be simultaneously obvious and complex. Not only does a healthy and nutritious diet allow us to grow and develop as children, but it also affects how we behave and learn in school, which in turn affects the employment opportunities and standards of living we have as adults. True to the insidious nature of structural racism, the ideal standard of upholding the right to food for all is not immune to racial inequities. For instance, household food insecurity has a strong influence on the academic success of high school students and their transition to higher education,⁵ an undeniable early foundation that paves the way for greater income security and subsequent food security during adulthood.5 However, PROOF (an interdisciplinary Canadian research consortium on food) found that 1 in 8 Canadian households were food insecure in 2017-18.⁶ Even more concerning, the prevalence of food insecurity within Indigenous- and Black-identified households (28.2% and 28.9%, respectively) was almost triple the prevalence of food insecurity amongst White-identified households (11.1%).⁶ A host of factors might explain these disparities, including racialized differences in income, the accessibility of quality and affordable food retailers in the neighbourhood, and housing stability.  Unfortunately, COVID-19 has only exacerbated such inequities. Shortly after the pandemic began, Statistics Canada data highlighted a clear racialized unemployment gap, with visible minority populations facing significantly higher (and in some cases, almost double) rates of unemployment than individuals not of a visible minority or Indigenous identity.⁷ With greater unemployment rates impacting income security for people of colour, the domino effects on household- and community-level food insecurity are not far behind. And so the story of food injustice continues – racial inequities in one system, such as access to economic opportunities, perpetuate inequities in the availability of and access to nutritious foods essential to our health and wellbeing. Once we begin to recognize structural racism within the very systems we inhabit, the natural next step is to identify what can be done, especially given the apparent amplification of inequities tied to the current pandemic. Recognizing the complexity behind structural racism and food security in Canada is a good start, but the purpose of recognition is not complacency. Rather, we must interrogate why such racial inequities exist, whether it be disparities related to job security or the disproportionate levels of racialized communities living in lower income neighbourhoods that lack access to affordable healthy foods.  Even in the mere act of reading these words, there is an inherent privilege and power you hold. Whether you are a student pursuing higher education, or a working professional browsing the web on your downtime, you have a voice and the agency to bring attention to these injustices. As with other sociocultural inequities in health and wellbeing, racialized food injustice and insecurity is an evident problem, but it is also an opportunity. An opportunity to start talking, questioning, and finding ways to act to implement comprehensive solutions that can help push our society towards equitable outcomes in health, wellbeing, and quality of life for all. References:
 The CHAIM Centre recognizes that the month of February celebrates Black excellence and resilience. At the same time, we are aware that systemic racism remains a pervasive issue in our society, with serious implications for the health of Black Canadians. This month and every month, as a research centre whose goal is to advance health research and its application to health care accessibility across Canada, we stand in alliance with Black students, colleagues, and community members to bring about the fundamental changes needed for a just and equitable society. In recognition of Black History Month, our team has compiled a reading list of articles that we personally found compelling on the topic of Black health and wellness. Many (but not all) of these articles focus on a Canadian perspective. ‘It just weighs on your psyche’: Black Americans on mental health, trauma, and resilience By: Crystal Milner An article featuring photos and interviews of Black Americans and their experiences and perspectives surrounding COVID, police brutality, and most importantly resilience. Police Brutality in Canada: A Symptom of Structural Racism and Colonial Violence By: Krista Stelkia This article by the Yellowhead Institute discusses how police brutality against Black and Indigenous people is the result of structural racism in Canadian society and the roles that policy, data, and solidarity have to play in holding our systems accountable. Untangling racism: Stress reactions in response to variations of racism against Black Canadians By: Kimberly Matheson et al. This academic article considers various aspects of the racism (e.g., extent of ambiguity or violence) that is encountered by Black Canadians, and the implications for stress-related emotional reactions, such as distress or anger. These emotional reactions have implications for vulnerability or resilience to depressive symptoms. Beyond Allyship: Motivations for Advantaged Group Members to Engage in Action for Disadvantaged Groups By: Helena Radke et al. Why do Whites participate in the BLM movement? There are several motivations for such allied action, some of which are authentic, and some that give rise to greater tension. This article reviews the research to understand the actions of allies. Taking Black Pain Seriously By: Oluwafunmilayo Akinlade Centering on the issue of pain treatment, this article from the New England Journal of Medicine is compelling, readable, and effectively illustrates the connection between the history of medical racism and current healthcare outcomes for Black patients. The Impact of COVID-19 on Black Canadians By: The African-Canadian Civic Engagement Council and Innovative Research Group The data in this report paints a clear and urgent picture of the disproportionate impact that the pandemic is having on Black communities in Canada, examining both health and financial trends related to COVID-19. Black History Month: Food For Thought (It’s Not What You Think) By: Jessica DeGore This article discusses emancipation in the American south, traditionally ‘poor’ southern food and how freedom affects cuisine. It explores how Black people throughout history used food and simple ingredients to create staples that persist today. Stop Whitewashing Our National History By: Tayo Bero Published in summer 2020, this article explores how Canada's failure to reckon with its historical mistreatment of Black and Indigenous people prevents us from addressing the racism embedded in Canadian society. Reparations as a Public Health Priority: A Strategy for Ending Black–White Health Disparities By: Mary T Bassett and Sandro Galea This article discusses the roots of the Black-White health gap in America, how this impacts access to medical resources, and how reparations could be leveraged to address this major disparity. Let's Talk: Whiteness and Health Equity By: National Collaborating Centre for Determinants of Health Aimed at a public health audience, this publication explains how "the practices, policies and perspectives that create and enable the dominance of White people, norms and culture" impacts the health of all Canadians, and presents strategies for disrupting Whiteness at the individual, institutional, and systemic levels to increase health equity. Urban renewal has displaced Black communities in Canada in the past. Can getting involved early in the planning stop it from happening again? By: Donovan Vincent This article discusses the impact that current and historical gentrification has had on Black communities in Canada. A group of experts weigh in on strategies to mitigate its effects. More Resources: A free 30-day course on allyship with prompts and reflections to act and think in solidarity with Black women. |
Archives
March 2023
Categories
All
|
 RSS Feed
RSS Feed